THYROID PHYSIOLOGY PART 1
1.
What are the hormones of thyroid gland?
From thyroid follicules 3
hormones
·
2
biological active – thyroxine = 3,5,3',5’-
tetraidothyronine (T4) and
3,5,3'-triiodothyronine (T3).
·
1 biologically inactive – rT3 (reverse T3)
2.
How do T3 and T4 differ structurally?
·
T3 and T4 consist of a phenyl ring attached via
an ether linkage to a tyrosine molecule.
·
Both have two iodine atoms on their tyrosine
(inner) ring.
·
They differ in that T4 has two iodine atoms on
its phenyl (outer) ring, whereas T3 has only one.
3.
How does rT3 differ from T3?
·
rT3
has 1 iodine in inner ring and 2 iodines in outer ring which is contrasting to
T3 which has 2 iodine in inner ring and 1 iodine in outer ring.
·
No
biological activity of rT3
·
rT3
levels can increase during illness and new born period.
4.
What are the sources of iodine?
Sea foods see weeds, vegetables and
sea salt. Iodination of salt is done in many countries
5.
Iodine reaches the thyroid gland in Iodide
form (I-).
6.
What is iodine pool?
It is the store of iodine in
extracellular fluid consisting of dietary
iodine, iodide released from the thyroid and by extrathyroidal deiodination of
the iodothyronines.
7. What is the daily recommended dietary allowance of iodine?
·
For
infants – 110 to 130 mcg
·
For
children – 90 to 120 mcg
·
For
adolescents and adults – 150 mcg
8.
How can we determine iodine deficiency?
By
urinary iodine excretion, as follows: mild iodine deficiency, 50 to 99 mcg/L;
moderate iodine deficiency, 20 to 49 mcg/L; and severe iodine deficiency,
<20 mcg/L.
9.
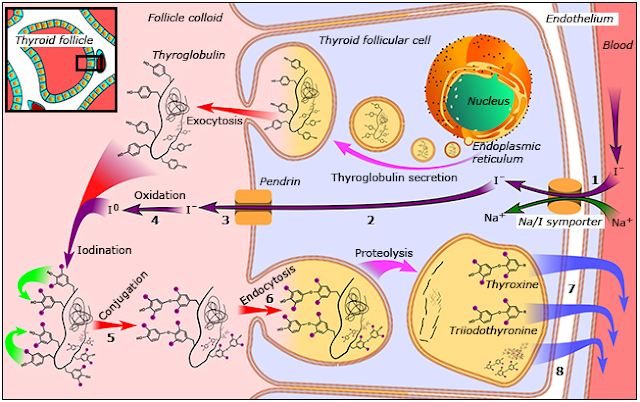
What are the steps of thyroid hormone
synthesis?
·
Transport
of iodine into thyroid
·
Oxidation
of iodine
·
Organification
·
Coupling
of iodinated tyrosine
·
Endocytosis
of iodinated tyrosine and release.
10. How
is iodine transported to thyroid ?
·
It
is located in basolateral membrane
·
It
is transported by a NaI symporter (NIS)
·
It
is an active transport process requiring ATP
·
It
transports I against electrical and chemical concentration gradient
·
Thyroid
gland has very high affinity for I and is able to trap I with a gradient of
100:1 relative to ECF
·
The
no of NIS increase in hypothyroidism and decreases in hyperthyroidism
·
Mutation
of NIS can cause hypothyroidism but is rare.
Other ions such as perchlorate and pertechnetate
also are transported into the thyroid by the same mechanism and, therefore, are
competitive inhibitors of iodide transport
11. Iodine
taken up by follicular cell diffuses towards apical membrane.
12. How
is iodine transported from apical membrane
to colloid?
·
It
is transported with help of pendrin transporter.
·
It
is I-Cl co-transporter
Mutation of the pendrin gene causes Pendred syndrome, a disorder
characterized by defective organification of iodine, goiter, and sensorineural
deafness.
13. What
is organification ?
·
After
diffusion of I into colloid oxidation of
I occurs and then it is covalently linked with one of the tyrosine residues of
thyroglobulin this process is organification.
·
Organification
is catalysed by enzyme Thyroid peroxidase (TPO) in the presence of Hydrogen
peroxidase
·
Hydrogen
peroxidase is produced by DUOX2(dual oxidase) the expression of which depends
on DUOXA2.
14. How
coupling occurs ?
·
The
coupling is binding of Monoidotyrosine (MIT) and Diodotyrosine(DIT) residues in
thyroglobulin.
·
When
2 DIT bind T4 is formed and when 1 MIT and 1 DIT bind T3 is formed.
·
This also requires TPO enzyme.
15. To
liberate T4 and T3, thyroglobulin is resorbed into the thyroid follicular cells
in the form of colloid droplets. The droplets fuse with lysosomes to form
phagolysosomes, in which the thyroglobulin is hydrolyzed to T4, T3, and its
other constituent amino acids, and some T4 is converted to T3. The hormones are
then secreted into the extracellular fluid and enter the circulation.
16. RECYLING OF IODINE
The
iodotyrosines liberated from thyroglobulin are deiodinated by iodotyrosine
deiodinase.
Most
of the iodide is then recycled for thyroid hormone synthesis.
Homozygous mutations in DEHAL1, the gene that encodes iodotyrosine deiodinase result in
iodotyrosine deiodinase deficiency with hereditary and sometimes severe
hypothyroidism and goiter.
17. What
is thyroglobulin?
·
It
is a 660kDa glycoprotein with 138 tyrosine residues.
·
It
is synthesized in ER
·
Normal thyroglobulin contains approximately six
molecules of monoiodotyrosine, four of diiodotyrosine, two of T4, and 0.2 of T3
per molecule.
18. In
adults thyroid gland secretes 85mcg of T4 and and 6-7 mcg of T3.
19. What
are the sources of T3?
80% of T3 is synthesized from T4
by peripheral conversion
20% from thyroid gland.
20. How
is T4 converted to T3?
It is converted by iodotyrosine
deiodinase.
21. What
are the types of iodotyrosine deiodinase?
3 types
·
Type I T4-5'-deiodinase is the predominant
deiodinating enzyme in the liver, kidney, and thyroid.
·
Type 1 is sensitive to propylthiouracil
·
Type II T4-5'-deiodinase is the predominant
deiodinating enzyme in muscle, brain, pituitary, skin, and placenta.
·
Type 2 is insensitive to propylthiouracil.
22. Which
organs have highest deiodinase activity ?
Kidney and liver.
23. In
a normal person T3 from Type 2 deiodinase comprises of 65% of T3.
24. Which
Deiodinase enzyme has higher affinity for T4?
Type 2
25. Which
enzyme gets highly activated during hypothyroidism?
Type 2 thus producing high T3 in
brain.
26. What
is the function of Type 3 deiodinase ?
·
Conversion
of T4 to rT3.
·
It
is active only during sick euthyroid
illness.
·
Massive
hemangiomas that express type III deiodinase are a rare cause of consumptive
hypothyroidism in infants.
A single nucleotide polymorphism in the type I
deiodinase (rs2235544) appears to increase deiodinase function, resulting in
higher ratios of free T3/free T4 in patients, including those taking T4 (levothyroxine).
A polymorphism in the type 2 deiodinase (rs225014)
may be associated with lower T3 concentrations and compromised psychological
well-being in treated hypothyroid patients, and a favorable response to
combined therapy with T4 and T3 (liothyronine).
27. What
is the role of selenium?
·
The deiodinases are selenoproteins, and the
thyroid has more selenium per gram of tissue than any other organ.
·
Selenium deficiency has been shown to
exacerbate both autoimmune thyroid disease and endemic cretinism.
28. How
is T4 metabolised ?
T4 is degraded by 10 percent
everyday.
80% are deiodinated === 40% to T3
and 40% to rT3
20% is conjugated with
glucoronide and sulfide.
29. Is
the peripheral conversion of T4 to T3 regulated by pituitary thyroid axis?
NO. it is independent.
30. Which
is the biologically active form?
T3. It binds with thyroid
receptor with 10-15 times more affinity than T4.
31. How
are Thyroid hormone distributed in the body.
|
T4 Distribution |
T3 distribution |
|
Free T4 0.02% (2ng/dl) |
Free T3 0.5% (0.4ng/dl) |
|
Lipoproteins 3% |
Lipoproteins 3% |
|
Albumin bound 12% |
Albumin bound 12% |
|
Transthyretin bound 10% |
Transthyretin bound 5% |
|
Bound to TBG 75% |
Bound to TBG 80% |
32. What
is the function of TBG?
It acts as both buffer and
storage of thyroid hormones.
33. TBGs
have higher affinity for T4 which may be the cause of longer half life of T4
about 7 days compared to 18 hours of T3
34. Also
the fraction of FT3 is higher than FT4 but the T3 is produced less from thyroid
the absolute value is less.
35. Unbound
or free thyroid hormones are biologically active form which remains constant
despite the increase or decrease of TBGs.
36. In
case of hypothyroidism the TBGs act as reservoir liberating free hormones until
the hormone are fully exhausted.
37. How are thyroid hormone
transported inside cells?
By
active transport and diffusion
The
monocarboxylate transporters MCT8 and MCT10 are involved in the transport of T4
and T3 (as well as reverse T3 (rT3).
38. What
is Allan-Herndon-Dudley syndrome?
It
is a X linked disorder causing mutations in MCT8 resulting in a severe
neurologic syndrome.
It
is characterized by low T4,high T3 and normal TSH.
39. Extrathyroidally where is the
maximum concentration of T3?
Intracellularly
40. What is the type of receptor for
thyroid hormone?
Nuclear receptor
Steroid receptor family
CLICK HERE FOR NEONATAL GRAVES
Dr. Nischal Neupane





Comments
Post a Comment