PHENYLKETONURIA
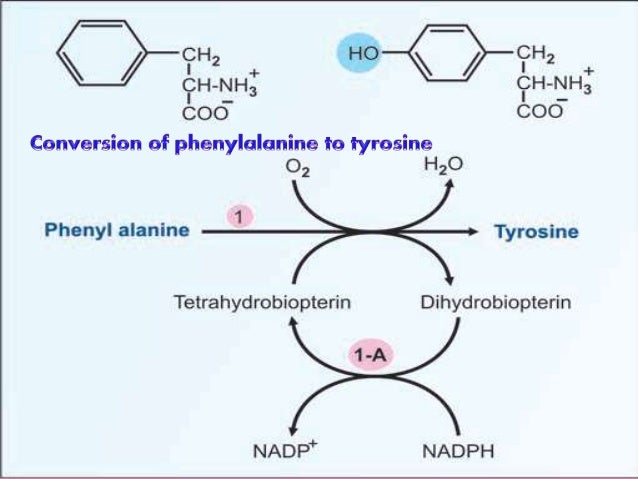
Phenylalanine is an essential amino acid.
Excess of phenylalanine which is not utilized by our body for protein synthesis is normally degraded by Tyrosine pathway.
How does phenylketonuria develop?
If there is deficiency of the enzyme phenylalanine hydroxylase (PAH) or of its cofactor tetrahydrobiopterin (BH4) then there will be accumulation of phenylalanine in body fluids & brain.
The severity of hyperphenylalaninemia depends on the degree of enzyme deficiency .
The levels of phenylalanine may vary from very high plasma concentrations ( >20 mg/dL, classic phenylketonuria [PKU] ) to mildly elevated levels, hyperphenylalaninemia (2-6 mg/dL).
In affected infants with plasma concentrations >20 mg/dL.
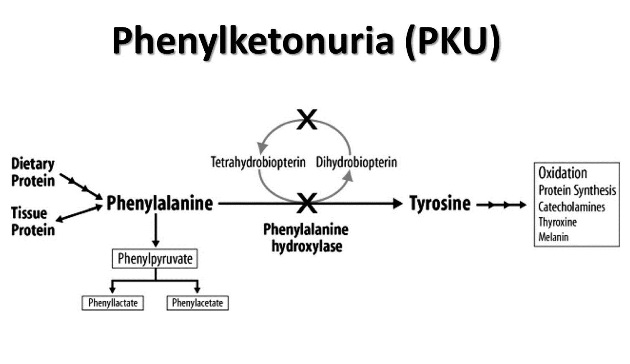
Excess phenylalanine is metabolized to Phenylketones (Phenylpyruvate and Phenylacetate) which is excreted in the urine (giving rise to the term phenylketonuria (PKU).
Which organ is mainly affected by hyperphenylalaninemia?
Brain
High concentration of phenylalanine in brain tissue is the cause of CNS damage.
Cerebral uptake of other amino acids like tyrosine and tryptophan are inhibited as the transport system is saturated by high levels of PKU.
Pattern of Inheritance
All defects causing hyperphenylalaninemia are inherited as autosomal recessive traits.
Prenatal diagnosis is possible using specific genetic probes in cells obtained from chorionic
villi biopsy.
What are the clinical features of Classic Phenylketonuria?
(Plasma phenylalanine levels >20 mg/dL)
The affected infant is normal at birth.
Profound mental retardation develops gradually if the infant remains untreated.
Cognitive delay may not be evident for the 1st few months.
In untreated patients, 50-70% will have an IQ below 35, and 88-90% below 65.
Only 2-5% of untreated patients will have normal intelligence.
Vomiting, sometimes severe enough to be misdiagnosed as pyloric stenosis, may be an early
symptom.
Older untreated children become hyperactive with autistic behaviors, including purposeless
hand movements, rhythmic rocking, and athetosis.
The infants are lighter in their complexion than unaffected siblings.
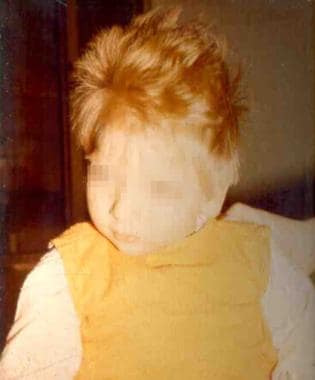
Some may have a seborrheic or eczematoid rash,(mild and disappears as the child grows older).
These children have an unpleasant MUSTY or MOUSEY odour of phenylacetic acid.
Neurologic signs :
Seizures (≈25%), spasticity, hyperreflexia, and tremors.
More than 50% have EEG abnormalities.
Microcephaly, prominent maxillae with widely spaced teeth, enamel hypoplasia, and growth
retardation.
What are the clinical features of milder Forms of Hyperphenylalaninemia /Non-PKU Hyperphenylalaninemias(Plasma phenylalanine levels >2 mg/dL,but <20 mg/dL)?
These infants do not excrete phenylketones.
But may still require dietary interventions.
Possibility of deficiency of BH4 should be investigated in all infants with the milder forms of
hyperphenylalaninemia.
How do we diagnose PKU?
Usually diagnosed through Newborn screening.

If screening is positive, diagnosis should be confirmed by quantitative measurement of plasma
phenylalanine concentration.
Identification and measurement of phenyl ketones in the urine has no place in any screening program.
In countries where such programs are not in effect, identification of phenylketones in the urine by ferric chloride may offer a simple test for diagnosis of infants with developmental and neurologic abnormalities.
Once hyperphenylalaninemia is diagnosed, additional studies for biopterin metabolism should
be performed to rule out biopterin deficiency as the cause of hyperphenylalaninemia.
Neonatal Screening for Hyperphenylalaninemia :
The method of choice is Tandem mass spectrometry , which identifies all forms of hyperphenyalaninemia with a low false-positive rate, and excellent accuracy and precision.
Diagnosis must be confirmed by measurement of plasma phenylalanine concentration.
Blood phenylalanine in affected infants with PKU may rise to diagnostic levels as early as 4 hr after birth even in the absence of protein feeding.
It is recommended that the blood for screening be obtained in the FIRST 24-48 hr of life after feeding protein to reduce the possibility of false-negative results, especially in the milder forms of the condition.
Treatment of PKU
The goal of therapy is to reduce phenylalanine levels in plasma & brain.
Formulas low in or free of phenylalanine should be given
The diet should be started as soon as diagnosis is established.
Because phenylalanine is not synthesized endogenously, small amounts of phenylalanine should be added to the diet to prevent phenylalanine deficiency.
Tyrosine becomes an essential amino acid in this disorder and its adequate intake must be ensured.
Plasma phenylalanine levels to be maintained:
In neonates through 12 yr of age: Between 2 - 6 mg/dL
In older individuals: Between 2 - 10 mg/dL
Discontinuation of therapy, even in adulthood, may cause deterioration of IQ and cognitive performance. Therefore phenylalanine-restricted diet should be continued for life.
Oral administration of Tetrahydrobiopterin (BH4) may result in reduction of plasma levels of phenylalanine in some patients with PAH deficiency.
Sapropterin, a synthetic form of BH4 is approved by the Food and Drug Administration (FDA) to reduce phenylalanine levels in PKU.
Hyperphenylalaninemia due to Deficiency of the Cofactor BH4
In 1-3% of infants with hyperphenylalaninemia, the defect resides in 1 of the enzymes necessary for production or recycling of the cofactor BH4
If these infants are misdiagnosed as having PKU, they may deteriorate neurologically despite adequate control of plasma phenylalanine.
In addition to acting as a cofactor for PAH, BH4 is also a cofactor for tyrosine hydroxylase and tryptophan hydroxylase, which are involved in the biosynthesis of dopamine and serotonin.
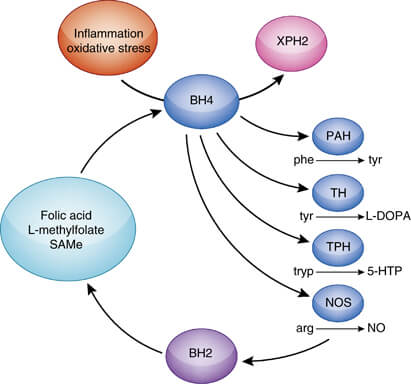
Therefore, patients with hyperphenylalaninemia due to BH4 deficiency also manifest neurologic findings related to deficiencies of the neurotransmitters dopamine and serotonin.
How do clinical features of PKU differ from neurotransmitter disorder?
Clinical manifestations of the neurotransmitter disorders differ greatly from those of PKU.
Neurologic symptoms of the neurotransmitter disorders often manifest in the 1st few months of life.
Include extrapyramidal signs with choreoathetotic or dystonic limb movements, axial and truncal hypotonia, hypokinesia, feeding difficulties, and autonomic problems.
Mental retardation, seizures, hypersalivation, and swallowing difficulties are also seen.
The symptoms are usually progressive and often have a marked diurnal fluctuation.
How do we proceed for diagnosis in case of BH4 deficiency cases?
Measurement of neopterin and biopterin in body fluids, especially urine.
In addition, examination of cerebrospinal fluid (CSF) reveals decreased levels of dopamine, serotonin, and their metabolites in all patients with BH4 deficiency.
BH4 loading test
Enzyme assay: The activity of dihydropteridine reductase can be measured in the dry blood spots on the filter paper used for screening purposes.
How do we treat cases of BH4 deficiency?
The goals of therapy are:
To correct hyperphenylalaninemia, and
To restore neurotransmitter deficiencies in the CNS.
Plasma phenylalanine should be maintained as close to normal
as possible (<6 mg/dL).
This can be achieved by a combination of a low phenylalanine diet and oral supplementation of BH4
Lifelong supplementation with neurotransmitter precursors such as L-dopa and 5-hydroxytryptophan, along with carbidopa.
Supplementation with folinic acid in patients with dihydropteridine reductase deficiency.
Some drugs such as trimethoprim-sulfamethoxazole,methotrexate, and other antileukemic agents are known to inhibit dihydropteridine reductase enzyme activity and should be used with great caution in patients with BH4 deficiency.


Comments
Post a Comment